“The patient is at peace, and the family is relieved.”
When a 15-year-old girl died in the palliative care center of Shougang Hospital, the family was not dissatisfied, but sent a pennant to express their gratitude. Since the launch of the palliative care pilot, patients with terminal diseases have a place to go, and some hospitals have ushered in new developments.
Behind the results, a group of caring medical staff are actively seeking to achieve more humanized medical services throughout the life cycle. At the same time, many problems such as imbalance between revenue and expenditure, personnel loss, and imperfect system also plague hospitals that “eat crabs” first.
How can palliative care go further?
Where does the funding come from?
Since the pilot, some hospitals have seized the opportunity to carry out palliative care: tertiary hospitals are committed to leading the direction of discipline construction, secondary hospitals are seeking survival in transformation, and primary hospitals are seeking differentiated development. Some hospitals have increased their popularity due to the outstanding level of palliative care business.
However, the heads of the palliative care teams of more than 10 hospitals in Beijing and Sichuan all said that their palliative care business is currently struggling to make ends meet.
According to a number of relevant persons in charge, at present, the charging and evaluation standards of the medical system are based on curative treatment, medical expenses are charged according to treatment items, and the cure rate is the core evaluation index. However, palliative care is care-centered, with few treatment items, and the core humanistic care items cannot be charged, nor can they cure patients.
“It can be expensive.” When applying to the hospital to carry out palliative care business, Qin Yuan, director of the palliative care department of Beijing Haidian Hospital, emphasized. Based on the responsibility of meeting the needs of residents in the jurisdiction, in 2017, Haidian Hospital established a palliative care ward with 6 beds. As demand increased, in 2022, palliative care became a separate specialty, with the number of beds increasing to 50.

Nurses’ Station of Palliative Care Center of Haidian Hospital. Photo by People’s Daily Chen Yexin
According to Qin Yuan, the hospital positions palliative care as a public welfare department, with an annual subsidy of more than 3 million yuan for 6 beds. With the increase in the number of beds, this model can no longer support the development of the department.
In March 2024, under the coordination of the Haidian District Party Committee, Haidian Hospital took the lead in trying to charge for non-medical service items, with a palliative care service fee of 200 yuan per day, and aromatherapy and other services on a per-time basis. Qin Yuan said that after the implementation of the new charging standard, the beds are still full, “with the team overloaded, the department’s income and expenditure are barely equal, but this situation is not sustainable.” ”
In November 2024, the National Health Insurance Administration (NHSA) issued the “Guidelines for the Establishment of Price Projects for Comprehensive Diagnosis and Medical Services (Trial)”, adding palliative care fees for the reference of provincial medical insurance bureaus and formulating a unified price benchmark for the whole province.
“This is a great support for the development of the industry.” Qin Yuan said that for the sake of safety, the charging standard set by Haidian Hospital was lower than the cost. “It’s important that the pricing can cover the cost and keep the department alive.”
Deyang City, Sichuan Province, is one of the first batch of pilot cities. In order to support the development of palliative care, in 2018, Deyang took the lead in piloting daily payment per bed, and patients no longer have to pay the minimum amount of basic medical insurance. In 2020, Deyang will also try to charge for non-medical service items, and hospitals can charge service fees.
The heads of the palliative care teams of the three surveyed hospitals in Deyang all said that there has been no charge for non-medical services. Yu Yuanfeng, deputy director of the palliative care ward of Deyang Hospital of Integrated Traditional Chinese and Western Medicine, said that palliative care patients can choose to pay per bed day or according to disease score (DIP), because both methods have limits, they cannot cover the cost of medical items, and non-medical service items can no longer be charged.
Yu Yuanfeng found that paying per bed day is more beneficial to most patients, but it will increase the burden on hospitals. The maximum reimbursement standard for medical insurance per bed day is 320 yuan, and the actual cost incurred by the patient is doubled, and the difference is borne by the hospital.
The reporter learned that the number of hospitals that actually carry out palliative care business in many places is less than the number of registered ones, one of the reasons is that there is an imbalance between revenue and expenditure, which is unsustainable. Most of the palliative care services that can be maintained are dependent on oncology, pain or geriatrics, etc., and the costs are shared. A small number of independent departments are given performance tilt by the hospital.
In order to formulate a scientific and reasonable medical insurance policy, the Health Commission, the Medical Insurance Bureau and other relevant departments in Beijing, Sichuan and other places have visited the hospital for many times to investigate and calculate the data.
“It’s not just a medical issue, there should be more people involved.” Lu Guijun, head of the palliative care team at Beijing Tsinghua Chang Gung Hospital, believes that the top priority is to integrate resources.
How do you retain talent?
“I also want to be a person with feelings.” Inspired by the pioneers, in 2020, Yu Yuanfeng participated in a week-long palliative care seminar in Beijing. She felt that the teacher spoke very well, but when she came back, she found that some of the ideas did not know how to put into practice.
A grandfather wants to see his grandson on his deathbed. Without being fully prepared, the grandson was frightened by the appearance of his grandfather. After walking out of the ward, the grandson said to Yu Yuanfeng, “Auntie, I’m afraid. She didn’t know how to reassure him, “I felt so helpless at the time.” ”
In 2023, she will study in Beijing again and feel that her ability to counsel and communicate with patients and families has been greatly improved.
The study also made her feel the power of a team, where a multidisciplinary team of doctors, nurses and social workers worked together to serve a patient, and everyone showed their strengths and complemented each other. “I can find other people for things I can’t do, and I solve problems that others can’t solve, which is where my value lies, and I feel full of energy.”
Yu Yuanfeng’s experience is a portrayal of many medical staff, and short-term theoretical study is not enough to train qualified palliative care practitioners. The palliative care department is facing difficulties in recruiting and retaining people.
Due to the fact that few medical schools offer relevant courses, many palliative care recruiters often have to “pick up the gaps” from other specialties and need to start training from scratch. Even if it is an old doctor, it takes at least half a year of training and practical operation to gradually change the concept.
Respondents said that the current talent training is mainly undertaken by hospitals with outstanding palliative care business. “In the long run, doing a good job in discipline construction is the foundation for solving the talent dilemma.” Qin Yuan said that palliative care involves the whole course of the disease, the whole spectrum of diseases, and all ages, which belongs to the branch of medicine, and medical treatment and medical education need a complete supporting system to support the long-term development of palliative care.
Even if you find someone who matches your philosophy, promotion is another hurdle. Qin Yuan said that it is very difficult for the palliative care department of Haidian Hospital to recruit medical staff.
As early as 2021, the current deputy director, Li Changhong, was interested in the palliative care department, but it was not until 2023 that she was successfully promoted to chief physician before she transferred to the department.
The palliative care team consists of doctors from a variety of specialties such as geriatrics and general practice. Li Changhong introduced that because palliative care has not yet established a specialty, there is no corresponding professional promotion channel for palliative care doctors to evaluate their titles.
The palliative care unit of Deyang Hospital of Integrated Traditional Chinese and Western Medicine is located in the geriatric department. Yu Yuanfeng is the deputy director of the geriatric department, and the title of the geriatric department is evaluated. Due to the long time it took to see palliative care patients, her associate chief physician review was stuck on the number of consultations. “The requirement is to reach 300 outpatient clinics and 8,000 patients.” She said that according to the prescribed job title every five years, she only saw 4,000 patients in eight years.
Compared with other specialties, palliative care has a thorough consultation and time-consuming communication, and the patient’s hospital stay is long and the patient’s condition changes greatly. “We have doctors who have been transferred to other departments and said that they would rather be in charge of 10 people there than 1 person here.” Yu Yuanfeng said.
Nursing teams face the challenges of long training times and frequent staff turnover. It takes 2-3 years to train a young nurse in the palliative care department, and many nurses leave due to high pressure and low salary. Deng Qian, deputy director of the palliative medicine department of West China Fourth Hospital, revealed that there is a frequent turnover of nurses in the department, “Our nurses do heavy work and get low wages, how can we keep people?” ”
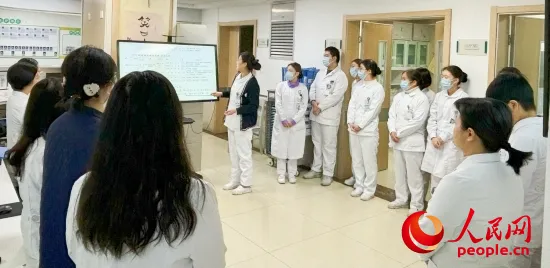
At the handover meeting of the Department of Palliative Medicine of West China Fourth Hospital, the nurse introduced the patient’s situation. Photo by People’s Daily reporter Jin Huihui
The provision of humanistic care and psychological support is a hallmark of palliative care, and medical social workers have an important role to play. The reporter learned that at present, there are a few palliative care teams with full-time social workers; Most hospitals cooperate with third-party organizations to hire part-time social workers, which is difficult to manage. There are also medical staff and social workers, but they are often inadequate.
“Medical technology is advancing, and if we can’t play a good role as social workers and volunteers, humanistic care is a big gap, and palliative care is still lame.” Deng Qian said.
How to effectively linkage?
Hospice care, palliative care, palliative care, etc. are collectively referred to as palliative care. Founded in 1995, the Department of Palliative Medicine of West China Fourth Hospital has explored a series of palliative care diagnosis and treatment techniques, guidelines and standardized clinical pathways in the past 30 years. In 2018, West China Fourth Hospital became a palliative care education and training center in Sichuan Province.
The diagnosis and treatment of refractory cancer pain is an important training content. According to Deng Qian, this is a mature technology, which has been mastered by more and more hospitals with the expansion of the training scale. “We’re exploring the experience of treating delirium. This is a common symptom in patients at the end of life, and sedation is difficult. ”
“Universal palliative care should be located in secondary and community hospitals, which are close to residents and more accessible.” Deng Qian believes that in the construction of the three-level linkage system of palliative care, tertiary hospitals should focus on critical and critical diseases, carry out education and training, build demonstration bases and guide lower-level hospitals, second-level hospitals to deal with mild cases, and first-level hospitals to do end-of-life care.
In 2018, Deyang Cancer Hospital, a tertiary hospital, established the Deyang Palliative Care Center with Deyang People’s Hospital in the form of a medical alliance and provided medical technology, quality control standards and patient referrals.
“This demonstrates the benefits of a three-tier triage system.” Liu Xiangfeng, deputy director of the Deyang Palliative Care Center, said that most of the patients in the center are from the Deyang People’s Hospital, and the hospital gives technical guidance to difficult problems such as refractory pain and psychological treatment.
The third batch of palliative care pilot projects requires the development of palliative care services in medical and elderly care institutions and community health service centers (township health centers), and encourages the development of home palliative care.
For the “novice” primary hospitals, drug restrictions and lack of diagnosis and treatment technology are the two major bottlenecks.
In 2022, Xinxing Health Center in Tianfu New Area, Sichuan Province officially launched palliative care services. Peng Xia, head of the hospital’s medical and elderly care department, said that the hospital can meet the palliative care needs of the elderly and surrounding residents, but the main problem encountered at present is that the procurement of drugs required for palliative care is limited under the constraints of the proportion of basic drugs.
“I didn’t dare to take in critically ill patients who carried multiple channels before, but now I have some confidence.” Zhong Chongxin, head of the sub-center of medical care and elderly care integration of Longhua Community Health Service Center in Longquanyi District, Chengdu, said that the guidance of the superior hospital made him full of confidence in the future development of palliative care, and hoped to solve the problem of drug restrictions and improve the level of diagnosis and treatment through the medical community.
Falling leaves are engraved in the cultural genes of Chinese people, and home palliative care responds to this demand.
Under the guidance of Shougang Hospital, the Jinding Street Community Health Service Center in Shijingshan District, Beijing, carried out home palliative care, but due to the shortage of manpower, the high cost of door-to-door visits, and the lack of standardization, the service of patients was limited. The Nanquan Town Health Center in Shifang City, Sichuan Province, is applying for a family hospital bed for palliative care, standardizing the door-to-door service process, fees and reimbursement standards, and exploring a new model of home palliative care.

The palliative care team of Shougang Hospital visits the patient. Photo by People’s Daily reporter Jin Huihui
The heads of the palliative care teams of many hospitals said that after the implementation of the three-level linkage, the turnover rate of beds in tertiary hospitals where it is difficult to find a bed has accelerated, the utilization rate of beds in primary and secondary hospitals has increased, and more and more patients in need have enjoyed palliative care services.
The “14th Five-Year Plan for the Development of National Aging Undertakings and Pension Service System” proposes that by 2025, each pilot city (district) and each county (city, district, banner) will set up at least one palliative care ward.
“If I could die like this, I would live better.” In the interview, many doctors, volunteers, patients and family members who know about palliative care have to say. More and more people are on the road, and although there are many questions to be solved, they believe that the future is long.

 Entering China
Entering China